Practice Essentials
Cancer of the esophagus remains a devastating disease because it is usually not detected until it has progressed to an advanced incurable stage. The most common types of esophageal carcinoma are squamous cell carcinoma and adenocarcinoma. There has been a steep increase in the incidence of esophageal adenocarcinoma, for which the most common predisposing factor is gastroesophageal reflux disease (GERD). It is estimated that in the United States, 21,560 people will be diagnosed with esophageal cancer and 16,120 will die of the disease in 2023. Of the new cases, it is estimated that 17,030 will occur in men and 4,530 in women. [1, 2, 3]
Modern multimodality precision imaging techniques, including barium esophagography, [4] contrast-enhanced computed tomography (CT), magnetic resonance imaging (MRI), endoscopic ultrasonography (EUS), [5] and positron-emission tomography (PET), are powerful tools in the detection, staging, diagnosis, and follow-up of esophageal carcinoma. [6, 7, 8, 9, 10, 11]
Endoscopic ultrasound (EUS) has become the standard technique for locoregional staging, with up to 90% accuracy in assessing tumor depth and locoregional and mediastinal lymph node. EUS allows fine-needle aspiration biopsy of suspicious lymph nodes (>1 cm) to confirm the presence of lymph node metastasis. Positron emission tomography CT (PET/CT) has become part of the routine pretreatment diagnostic workup. PET allows the detection of occult sites of distant metastatic spread. CT of the thorax and abdomen is performed to evaluate the extent of the primary tumor and to search for potential liver and lung metastases and retroperitoneal and mediastinal lymphadenopathy. [12]
In a study by Mantziari et al of 18F- FDG PET/CT-derived parameters of esophageal cancer for maximal standardized uptake value, total lesion glycolysis, and metabolic tumor volume, SUVmax greater than 8.25 g/mL, TLG greater than 41.7 g, and MTV greater than 10.70 cm3 were significantly associated with locally advanced cT3/4 stage. A baseline SUVmax greater than 12.7 g/mL was associated with early tumor recurrence and poor disease-free survival, particularly for squamous cell cancer. [13]
Because squamous cells line the entire esophagus, squamous cell carcinoma can occur in any part of the esophagus, but it often arises in the upper half of the esophagus. Adenocarcinoma typically develops in specialized intestinal metaplasia (Barrett metaplasia) that develops as a result of GERD and, therefore, typically arises in the lower half of the distal esophagus, often involving the esophagogastric junction.
(See the images below.)
 Nonenhanced axial CT image at the level of the origin of the great vessels demonstrates a nasogastric tube in place. The esophageal wall is thickened circumferentially and exerts mass effect on the posterolateral tracheal wall. Infiltration of the mediastinal fat adjacent to the great vessels is present. Findings are consistent with esophageal carcinoma with tracheal invasion.
Nonenhanced axial CT image at the level of the origin of the great vessels demonstrates a nasogastric tube in place. The esophageal wall is thickened circumferentially and exerts mass effect on the posterolateral tracheal wall. Infiltration of the mediastinal fat adjacent to the great vessels is present. Findings are consistent with esophageal carcinoma with tracheal invasion.
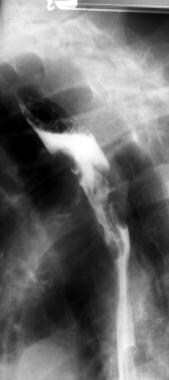
 Lateral barium esophagram demonstrates a large, intraluminal, lobulated filling defect diagnosed as esophageal carcinoma during endoscopic biopsy.
Lateral barium esophagram demonstrates a large, intraluminal, lobulated filling defect diagnosed as esophageal carcinoma during endoscopic biopsy.
Early detection remains the elusive but essential goal of research. Only surgical resection at a very early stage has been shown to improve survival rates in patients with this disease. [14] However, the recurrence rate after radical resection of esophageal cancer is reported to be approximately 50%, and most cases of recurrence occur within 2 years after surgery. Also, patients with esophageal squamous cell carcinoma have a high prevalence of second primary head and neck squamous cell carcinoma and require surveillance of the head and neck before treatment and at follow-up. [15]
Preferred examination
Endoscopic ultrasound (EUS) has become the standard technique for locoregional staging, with up to 90% accuracy in assessing tumor depth and locoregional and mediastinal lymph node. EUS allows fine-needle aspiration biopsy of suspicious lymph nodes (>1 cm) to confirm the presence of lymph node metastasis. [12]
Positron emission tomography CT (PET/CT) has become part of the routine pretreatment diagnostic workup. PET allows the detection of occult sites of distant metastatic spread. CT of the thorax and abdomen is performed to evaluate the extent of the primary tumor and to search for potential liver metastases and celiac lymphadenopathy, as well as other distant metastases. [12]
Computed tomography (CT) of the thorax and abdomen should be performed to evaluate the extent of the primary tumor and search for liver metastases and celiac lymphadenopathy. However, CT is inconsistent to differentiate tumor depth, has poor lymph node sensitivity, and may not detect small metastases, particularly within the peritoneum. [16, 8, 17, 18, 19, 20]
Barium esophagography is a useful initial examination in the evaluation of a patient with esophageal complaints, because it allows the assessment of esophageal morphology and motility. It can show a filling defect due to tumor or irregularity of the wall of the esophagus. Esophageal endoscopy permits direct inspection and biopsy of the esophageal mucosa for histologic diagnosis. For the purpose of staging esophageal carcinoma, endoscopic ultrasound (EUS), contrast-enhanced CT, and PET each offer unique information.
In a study of 375 patients with esophageal carcinoma after definitive treatment, the researches reported that the diagnostic sensitivity and specificity of PET/CT for detecting recurrent esophageal carcinomas were 100% (64/64) and 94.0% (675/718). [21, 22]
EUS is not necessary in patients with distant metastases or following preoperative (neoadjuvant) chemoradiotherapy. EUS is the most sensitive test to exclude local tumor invasion and regional nodal disease that would make endoscopic resection (ER) unsafe or unnecessary. For early esophageal cancer staging, EUS followed by ER and histopathologic analysis remains the standard of care. For a minority of locally advanced cancers, EUS fine-needle aspiration can define the radiotherapy field by providing tissue samples of suspicious lymph nodes that are remote from the primary tumor. [23]
Limitations of techniques
Barium esophagography has optimal sensitivity for the detection of lesions when a double-contrast technique is used. Such technique requires that the patient be able to stand upright, which may not be possible with patients who are debilitated. For bulkier obstructive lesions, an air-contrast technique may not be possible, and a detailed mucosal examination may not be achieved distal to the obstruction.
A notable limitation of CT in diagnosis involves the characterization of lymph nodes. With CT scans, size criteria are used to determine possible metastatic involvement; however, lymph nodes may be enlarged because of infectious or inflammatory etiologies. Conversely, subcentimeter lymph nodes may harbor metastatic tumor.
Ultrasonographic examinations are highly operator dependent. Limitations of EUS include an inability to pass the malignant stricture with the transducer. This limitation results in an incomplete examination. [24] However, the use of a dedicated 8-mm-diameter esophagoprobe for EUS allows complete examination in most patients.
With PET, the resolution and cost remain the primary limitations. Subcentimeter foci of tumor metabolism may not be detected.
Guidelines
The Society of Thoracic Surgeons clinical practice guidelines for esophageal cancer include the following [25] :
-
Flexible endoscopy with biopsy is the primary method for diagnosis of esophageal cancer.
-
CT of the chest and abdomen is optional for staging of early-stage esophageal cancer and recommended for staging locoregionalized esophageal cancer.
-
PET is optional for staging of early-stage esophageal cancer and recommended staging of locoregionalized esophageal cancer.
-
In patients without metastatic disease, endoscopic ultrasonography is recommended to improve the accuracy of staging.
-
In patients with small, discrete nodules or areas of dysplasia in whom disease appears limited to the mucosa or submucosa as assessed by endoscopic ultrasonography, endoscopic mucosal resection should be considered as a diagnostic/staging tool.
-
In patients with locally advanced (T3/T4) adenocarcinoma of the esophagogastric junction infiltrating the anatomic cardia or Siewart type III esophagogastric tumors, laparoscopy is recommended to improve the accuracy of staging.
The National Comprehensive Cancer Network has published guidelines on esophageal and esophogogastric junction cancers, including the following [26] :
-
EUS and FDG-PET/CT evaluation from skull base to midthigh is recommended if metastatic disease is not evident.
-
HER2, MSI-H/dMMR, and PD-L1 testing are recommended at the time of diagnosis if metastatic disease is documented or suspected.
-
Assessment of Siewert tumor type should be included as part of the initial workup in all patients with EGJ adenocarcinoma.
The European Society of Medical Oncology has published the following guidelines [27] :
-
Staging should include a complete clinical examination and a CT scan of the neck, chest, and abdomen.
-
In candidates for surgical resection, EUS should be carried out to evaluate the T and N tumor categories.
-
Fluorodeoxyglucose ( 18F) FDG-PET should be carried out in patients who are candidates for esophagectomy.
Radiography
Barium esophagography is unique among esophageal studies for assessing both morphology and motility. Barium esophagography remains the study of choice for characterization of esophageal strictures. Esophageal carcinoma may demonstrate a variety of appearances on barium esophagrams. The morphologic pattern of the lesion on barium esophagrams establishes the need to consider the differential diagnoses.
Lesions may be annular and constricting; intraluminal, polypoid, or masslike; infiltrative; ulcerating; or varicoid. A mixed pattern is most common. Early esophageal carcinoma may present as a small polypoid lesion or as coalescent plaques or nodules. A double-contrast technique should be used for optimal sensitivity.
The length and location of the involved esophageal segment and the functional impairment resulting from the lesion should be reported. Once a malignancy is detected on barium examination, the radiologist must be careful to evaluate the remainder of the esophagus and stomach for synchronous lesions. Endoscopy should follow.
(See the images below.)
 Anteroposterior barium esophagram demonstrates an abrupt change in the caliber of the esophagus, with a long, irregular, annular stricture of the thoracic esophagus. Note the masslike shouldering at the proximal extent of the lesion at which filling defects are present within the dilated esophageal lumen. Findings are most consistent with esophageal carcinoma.
Anteroposterior barium esophagram demonstrates an abrupt change in the caliber of the esophagus, with a long, irregular, annular stricture of the thoracic esophagus. Note the masslike shouldering at the proximal extent of the lesion at which filling defects are present within the dilated esophageal lumen. Findings are most consistent with esophageal carcinoma.
 Lateral barium esophagram demonstrates an abrupt change in the caliber and contour of the esophagus caused by an irregular circumferential stricture containing focal ulcerations. Findings are most consistent with esophageal carcinoma.
Lateral barium esophagram demonstrates an abrupt change in the caliber and contour of the esophagus caused by an irregular circumferential stricture containing focal ulcerations. Findings are most consistent with esophageal carcinoma.
 Lateral barium esophagram demonstrates marked irregular narrowing of the esophageal lumen with focal ulcerations and almost complete obstruction; these findings are consistent with esophageal carcinoma.
Lateral barium esophagram demonstrates marked irregular narrowing of the esophageal lumen with focal ulcerations and almost complete obstruction; these findings are consistent with esophageal carcinoma.
Levine et al reviewed 2484 barium esophagrams and found that endoscopy had been recommended in 26 patients (1%) because of findings suggestive of malignancy. Cancer was ultimately diagnosed in 11 patients, yielding a positive predictive value of 42%. The same investigators also retrospectively reviewed 50 cases of endoscopically proven esophageal carcinoma and found that lesions were present on barium esophagrams in 49 patients (98%). In addition, carcinoma was diagnosed or suggested in 48 patients (96%) on the basis of the barium study results. [28, 29]
Computed Tomography
Contrast-enhanced CT plays an important role in the staging of esophageal carcinoma. Attention is directed at determining the extent of the local tumor; invasion of mediastinal structures; involvement of supraclavicular, mediastinal, or upper abdominal lymph nodes; and distant metastases. These observations are useful in distinguishing between T3 and T4 lesions and in determining the N and M status.
CT examination should extend from the thoracic inlet through the liver. Routine oral contrast material should be administered, which may be a positive contrast agent, such as dilute barium, or a negative intraluminal contrast medium, such as water. A low-density 3% weight-for-weight esophageal barium paste may be administered immediately prior to scanning. Techniques for virtual esophageal endoscopy have also been described using effervescent granules and glucagon. [16, 8, 17, 18, 19, 20]
Multiple groups have reported on the sensitivity and specificity of CT in determining lymph node involvement. Its sensitivity for the detection of lymph node metastases is in the range of 60-80%. Its specificity is higher, approximately 90%.
An impression of tracheal invasion may be caused by expiratory bowing of the posterior trachea. Lymph node metastases may be present without enlarged lymph nodes, and lymph node enlargement may not be the result of malignancy. Lesions in solid organs identified at CT may represent primary benign or malignant processes or metastatic disease, and biopsy is frequently necessary to obtain histologic proof.
(See the images below.)
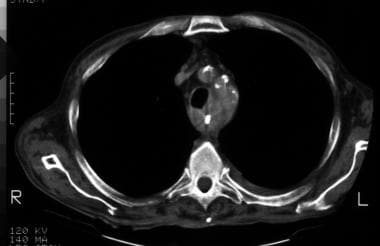
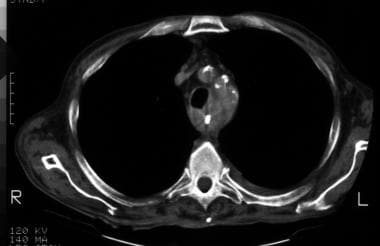 Nonenhanced axial CT image at the level of the origin of the great vessels demonstrates a nasogastric tube in place. The esophageal wall is thickened circumferentially and exerts mass effect on the posterolateral tracheal wall. Infiltration of the mediastinal fat adjacent to the great vessels is present. Findings are consistent with esophageal carcinoma with tracheal invasion.
Nonenhanced axial CT image at the level of the origin of the great vessels demonstrates a nasogastric tube in place. The esophageal wall is thickened circumferentially and exerts mass effect on the posterolateral tracheal wall. Infiltration of the mediastinal fat adjacent to the great vessels is present. Findings are consistent with esophageal carcinoma with tracheal invasion.
 Sagittal reformatted chest CT scan demonstrates marked, long-length, esophageal wall thickening abutting the posterior tracheal wall. Tracheal invasion by esophageal carcinoma was found at bronchoscopy.
Sagittal reformatted chest CT scan demonstrates marked, long-length, esophageal wall thickening abutting the posterior tracheal wall. Tracheal invasion by esophageal carcinoma was found at bronchoscopy.
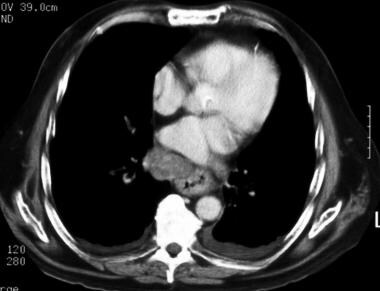 Enhanced axial CT image demonstrates irregular wall thickening of the esophagus. A heterogeneously enhancing mass to the right of the esophagus represents a markedly enlarged metastatic lymph node. No significant loss of the fat plane is noted between the esophageal mass and the descending thoracic aorta, indicating the absence of aortic invasion. Small bilateral pleural effusions are present.
Enhanced axial CT image demonstrates irregular wall thickening of the esophagus. A heterogeneously enhancing mass to the right of the esophagus represents a markedly enlarged metastatic lymph node. No significant loss of the fat plane is noted between the esophageal mass and the descending thoracic aorta, indicating the absence of aortic invasion. Small bilateral pleural effusions are present.
 Nonenhanced axial CT image demonstrates a large proximal esophageal mass with asymmetric impression on the posterior tracheal wall, suggestive of invasion. Recall that the posterior tracheal wall may bow inwardly (usually symmetrically) during expiration because of incomplete tracheal cartilage rings. Infiltration of the peri-esophageal fat is demonstrated, although no evidence of aortic invasion is present.
Nonenhanced axial CT image demonstrates a large proximal esophageal mass with asymmetric impression on the posterior tracheal wall, suggestive of invasion. Recall that the posterior tracheal wall may bow inwardly (usually symmetrically) during expiration because of incomplete tracheal cartilage rings. Infiltration of the peri-esophageal fat is demonstrated, although no evidence of aortic invasion is present.
 Enhanced axial CT image demonstrates a large esophagogastric junction carcinoma and several large liver lesions, with heterogeneous peripheral contrast enhancement and irregular margins consistent with metastases.
Enhanced axial CT image demonstrates a large esophagogastric junction carcinoma and several large liver lesions, with heterogeneous peripheral contrast enhancement and irregular margins consistent with metastases.
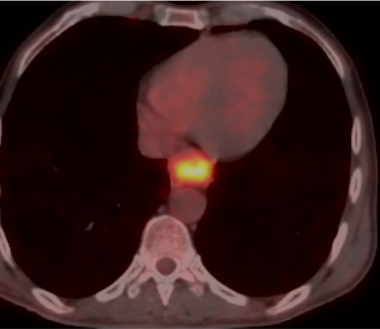
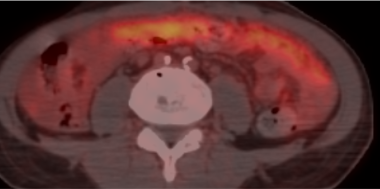
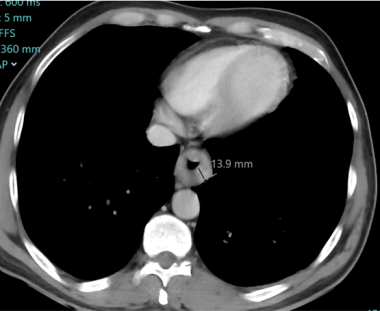 Axial enhanced CT scan of an 80-year-old man complaining of dysphagia showing circumferential thickening of the esophagus, narrowing the lumen without evidence of invasion of aorta. After medical treatment, symptoms improved, but three months later the symptoms aggravated and a repeat CT scan showed increased esophageal wall thickening, obliterating the lumen. Following this, a PET CT was obtained which confirmed the primary tumor and additionally showed peritoneal carcinomatosis.
Axial enhanced CT scan of an 80-year-old man complaining of dysphagia showing circumferential thickening of the esophagus, narrowing the lumen without evidence of invasion of aorta. After medical treatment, symptoms improved, but three months later the symptoms aggravated and a repeat CT scan showed increased esophageal wall thickening, obliterating the lumen. Following this, a PET CT was obtained which confirmed the primary tumor and additionally showed peritoneal carcinomatosis.
 Axial enhanced CT scan of an 80-year-old man complaining of dysphagia showing circumferential thickening of the esophagus, narrowing the lumen without evidence of invasion of aorta. After medical treatment, symptoms improved, but three months later the symptoms aggravated and a repeat CT scan showed increased esophageal wall thickening, obliterating the lumen. Following this, a PET CT was obtained which confirmed the primary tumor and additionally showed peritoneal carcinomatosis.
Axial enhanced CT scan of an 80-year-old man complaining of dysphagia showing circumferential thickening of the esophagus, narrowing the lumen without evidence of invasion of aorta. After medical treatment, symptoms improved, but three months later the symptoms aggravated and a repeat CT scan showed increased esophageal wall thickening, obliterating the lumen. Following this, a PET CT was obtained which confirmed the primary tumor and additionally showed peritoneal carcinomatosis.
A sample helical CT (single detector) protocol includes the intravenous administration of 150 mL of 60% contrast material injected at a rate of 2-3 mL/s with a scanning delay of 50 seconds after the start of the injection; a pitch of 1.5 and a 5-mm section thickness may be used. For multidetector-row CT, 100 mL of 60% intravenous contrast medium may be injected at a rate of 3 mL/s with a scanning delay of 40 seconds after the start of the injection; a pitch of 6 and a 2.5-mm section thickness may be used. [17]
CT scans should be obtained during full inspiration when patients are evaluated for esophageal carcinoma. Inward bowing of the trachea and mainstem bronchi during expiration may produce the false impression of tracheobronchial invasion. [18, 19]
Key findings include the following:
-
Eccentric or circumferential wall thickening is greater than 5 mm.
-
Peri-esophageal soft tissue and fat stranding may be demonstrated.
-
A dilated fluid- and debris-filled esophageal lumen is proximal to an obstructing lesion.
-
Tracheobronchial invasion appears as displacement of the airway (usually the trachea or left mainstem bronchus) as a result of mass effect by the esophageal tumor. Absence of a fat plane between the airway and the esophageal mass cannot be used as an indication of invasion. Even in patients without esophageal carcinoma, a fat plane is usually not evident between the esophagus and left mainstem bronchus.
-
Note that the tracheal cartilage rings are incomplete posteriorly, which allows the posterior wall of the trachea to bow anteriorly during expiration; therefore, it is important that CT images be acquired during full inspiration.
-
Aortic invasion may be assessed in 2 ways: (1)The Picus method considers the arc of contact between the tumor and aorta. [30] Loss of the periaortic fat plane of less than 45° suggests no aortic invasion, whereas contact of 90° or more is predictive of invasion of the aortic wall. Contact between 45° and 90° is indeterminate. Accuracy with this method is 80%. (2) Obliteration of the triangular fat space between the aorta, esophagus, and spine is another predictor of aortic invasion.
-
A careful search for lymph nodes is an essential component of the interpretation. A short-axis diameter exceeding 1 cm is considered abnormal for lymph nodes in all mediastinal locations except those in the subcarinal region, in which 1.4 cm is the upper limit of normal. Because lymph nodes may harbor metastases without being enlarged, noting the location of any identified lymph nodes is important. In addition, remembering that lymph nodes may be enlarged because of inflammatory or infectious etiologies is important.
-
Esophageal carcinoma is often metastatic at presentation.
-
In a review of 838 patients with M1 disease, Quint et al found that metastases were diagnosed most commonly in the abdominal lymph nodes (45%); liver (35%); lung (20%); cervical and/or supraclavicular lymph nodes (18%); bone (9%); adrenal glands (5%); peritoneum (2%); brain (2%); or stomach, pancreas, pleura, skin or body wall, pericardium, or spleen (1% each). The same group found that none of the cases with stage M0, as determined at chest and abdominal CT, were upstaged to M1 during either bone scanning or head CT. [31]
-
Reviewing a cohort of 116 cases of predominantly esophageal squamous cell carcinoma, Margolis et al determined that a solitary lung nodule found at the time of diagnosis is more likely to be a benign abnormality or a primary lung cancer than a metastatic lesion. [32] However, during terminal phases of the disease, lung metastases are increasingly common.
Magnetic Resonance Imaging
MRI presents the advantage of direct multiplanar imaging capabilities, which may be of particular use in assessing tracheobronchial, aortic, and pericardial invasion. MRI has not yielded other significant advantages when compared to CT in the staging of esophageal carcinoma.
Research studies suggest that T2-weighted MRIs obtained with an endoluminal coil can reveal 7 layers of the esophageal wall [33] :
-
Epithelial layer (intermediate intensity)
-
Lamina propria and muscularis mucosa (low intensity)
-
Submucosa (high intensity)
-
Inner circular muscularis propria (low intensity)
-
Intermuscular structure (high intensity)
-
Outer longitudinal muscularis propria (low intensity)
-
Subadventitial structures (high intensity)
Ultrasonography
Unlike CT, endoscopic ultrasonography (EUS) allows visualization of the distinct layers within the esophageal wall. Alternating circumferential layers define the mucosal interface (hyperechoic), the mucosa (hypoechoic), the submucosa (hyperechoic), the muscularis propria (hypoechoic), and the adventitial interface (hyperechoic). Such resolution permits the distinction of T1, T2, T3, and T4 tumors. Esophageal carcinoma appears as a hypoechoic lesion disrupting the normal circumferential layers. However, with standard EUS equipment, often only 3 layers are seen in the esophageal wall: the mucosa and submucosa (hyperechoic), the muscularis propria (hypoechoic), and the adventitial interface (hyperechoic).
Local lymph nodes are also demonstrated by using EUS. Nodes are considered malignant if they are round, if they are hypoechoic, and if they have well-defined borders. Usually, benign nodes are hyperechoic and less well defined.
T-stage accuracy with EUS is in the range of 79-94%. Accuracy is better for T3 or T4 lesions than for T1 or T2 lesions. N-stage accuracy is in the range of 69-90%. Distant metastases cannot be reliably identified with EUS because of the limited field of view. [24] According to Rasanen et al, the technique probably outperforms CT and PET in the detection of locoregional lymph node metastasis. [34]
Nuclear Imaging
PET is useful not only for the primary detection of tumor and metastases but also for the further characterization of abnormalities discovered by using other imaging modalities. [35, 36, 37] Fluorodeoxyglucose (FDG) is the most commonly used radiopharmaceutical. FDG is taken up by cells and trapped within them by means of phosphorylation. FDG decays inside the cell, with a half-life of approximately 110 minutes, while emitting positively charged electrons called positrons. A positron travels a short distance in tissue before colliding with an electron. Collision results in annihilation of the 2 particles and the emission of photons. The detection of the photons by using ring detectors is the basis for image formation. [38]
In a systematic review and meta-analysis, 18F-FDG and PET/CT were found to be a reliable imaging modality for detecting recurrent esophageal cancer after treatment. Pooled estimates of sensitivity and specificity for 18F-FDG PET or PET/CT in diagnosing recurrent esophageal cancer were 96% (95% confidence interval [CI]: 93-97%) and 78% (95% CI: 66-86%), respectively. According to the study, however, histopathologic confirmation of 18F-FDG or PET/CT suspected lesions was required because of a considerable false-positive rate. [39]
In a study by Mantziari et al of 18F- FDG PET/CT-derived parameters of esophageal cancer, SUVmax greater than 8.25 g/mL, TLG greater than 41.7 g, and MTV greater than 10.70 cm3 were significantly associated with locally advanced cT3/4 stage. A baseline SUVmax greater than 12.7 g/mL was associated with early tumor recurrence and poor disease-free survival, particularly for squamous cell cancer. [13]
Radiopharmaceuticals other than FDG can be used in PET imaging. Carbon-11 choline has received particular attention. Choline, a component of the cell membrane, is taken up by actively dividing cells.
In theory, this agent provides some advantages over FDG. Uptake of FDG requires that the tumor derive a portion its energy supply from glycolysis, an anaerobic condition that exists when the oxygen supply to some part of the tumor is low. For example, this circumstance may occur when a tumor outgrows its arterial supply. On the other hand, the uptake of 11C-choline requires only the presence of cell division. Cardiac uptake of FDG may be significant, even in the fasting state, and this characteristic complicates the interpretation of findings in the mediastinum. Conversely, cardiac uptake is not significant with 11C-choline.
C-11-choline PET scanning has been shown to outperform FDG-PET scanning in the detection of malignant mediastinal lymph nodes. With this agent, tumor-containing mediastinal lymph nodes as small as 4 mm have been identified. The short half-life of 11C-choline (approximately 20 min) will likely limit its use in major academic centers. The agent is not useful in the abdomen because of intense liver uptake. FDG-PET scanning remains the technique of choice for the detection of metastatic abdominal lymph nodes.
In a study of 375 patients with esophageal carcinoma after definitive treatment, the researches reported that the diagnostic sensitivity and specificity of PET/CT for detecting recurrent esophageal carcinomas were 100% (64/64) and 94.0% (675/718). [21]
Degree of confidence
Flamen et al performed a prospective study to compare the staging of esophageal carcinoma with FDG-PET versus the combination of CT and EUS in 74 patients. For T stages, FDG-PET scanning demonstrated increased activity in the primary tumor in 70 patients (95% sensitivity). Four proven T1 lesions had negative findings on FDG-PET scans. FDG-PET had a higher accuracy in diagnosing stage IV disease than CT and EUS combined; the results led to upstaging of the disease in 11 of 74 patients and downstaging of the disease in 5 of the patients. [40]
In a meta-analysis by Kroese et al, 18F-FDG PET/CT restaging after neoadjuvant therapy for esophageal cancer was shown to detect true distant interval metastases in 8% of patients and therefore considerably impacted treatment decision making. However, false positive distant findings occurred in 5% of patients at restaging with 18F-FDG PET/CT, underlining the need for pathologic confirmation of suspected lesions. [41]
The sensitivity of FDG-PET in assessing nodal metastasis is reportedly 33-83%, but studies have shown the superiority of FDG-PET to CT and EUS for determining the N status. FDG-PET is more sensitive than CT for the detection of distant metastases. [42]
Kobori et al have shown that the combination of FDG and 11C-choline PET allowed the identification of 85% of the cases with metastatic lymph nodes. [43]
FDG-PET scans may fail to demonstrate T1 primary lesions. Inflammatory processes cause increased uptake of FDG. In addition, patients with no esophageal pathology may have minimal esophageal FDG uptake, particularly in distal areas.
-
Anteroposterior barium esophagram demonstrates an abrupt change in the caliber of the esophagus, with a long, irregular, annular stricture of the thoracic esophagus. Note the masslike shouldering at the proximal extent of the lesion at which filling defects are present within the dilated esophageal lumen. Findings are most consistent with esophageal carcinoma.
-
Lateral barium esophagram demonstrates an abrupt change in the caliber and contour of the esophagus caused by an irregular circumferential stricture containing focal ulcerations. Findings are most consistent with esophageal carcinoma.
-
Lateral barium esophagram demonstrates marked irregular narrowing of the esophageal lumen with focal ulcerations and almost complete obstruction; these findings are consistent with esophageal carcinoma.
-
Oblique barium esophagram demonstrates a focal, fixed, concave contour deformity of the posterior esophageal wall. This represents superficial spreading esophageal carcinoma.
-
Lateral barium esophagram demonstrates a large, intraluminal, lobulated filling defect diagnosed as esophageal carcinoma during endoscopic biopsy.
-
Nonenhanced axial CT image at the level of the origin of the great vessels demonstrates a nasogastric tube in place. The esophageal wall is thickened circumferentially and exerts mass effect on the posterolateral tracheal wall. Infiltration of the mediastinal fat adjacent to the great vessels is present. Findings are consistent with esophageal carcinoma with tracheal invasion.
-
Sagittal reformatted chest CT scan demonstrates marked, long-length, esophageal wall thickening abutting the posterior tracheal wall. Tracheal invasion by esophageal carcinoma was found at bronchoscopy.
-
Enhanced axial CT image demonstrates irregular wall thickening of the esophagus. A heterogeneously enhancing mass to the right of the esophagus represents a markedly enlarged metastatic lymph node. No significant loss of the fat plane is noted between the esophageal mass and the descending thoracic aorta, indicating the absence of aortic invasion. Small bilateral pleural effusions are present.
-
Nonenhanced axial CT image demonstrates a large proximal esophageal mass with asymmetric impression on the posterior tracheal wall, suggestive of invasion. Recall that the posterior tracheal wall may bow inwardly (usually symmetrically) during expiration because of incomplete tracheal cartilage rings. Infiltration of the peri-esophageal fat is demonstrated, although no evidence of aortic invasion is present.
-
Enhanced axial CT image demonstrates a large esophagogastric junction carcinoma and several large liver lesions, with heterogeneous peripheral contrast enhancement and irregular margins consistent with metastases.
-
Axial enhanced CT scan of an 80-year-old man complaining of dysphagia showing circumferential thickening of the esophagus, narrowing the lumen without evidence of invasion of aorta. After medical treatment, symptoms improved, but three months later the symptoms aggravated and a repeat CT scan showed increased esophageal wall thickening, obliterating the lumen. Following this, a PET CT was obtained which confirmed the primary tumor and additionally showed peritoneal carcinomatosis.
-
Axial enhanced CT scan of an 80-year-old man complaining of dysphagia showing circumferential thickening of the esophagus, narrowing the lumen without evidence of invasion of aorta. After medical treatment, symptoms improved, but three months later the symptoms aggravated and a repeat CT scan showed increased esophageal wall thickening, obliterating the lumen. Following this, a PET CT was obtained which confirmed the primary tumor and additionally showed peritoneal carcinomatosis.
-
There is avid FDG activity at the primary tumor.
-
Diffuse thickening of the omentum (omental caking) with avid activity indicating peritoneal carcinomatosis.